
Daniel Peterschmidt
A version of this story originally appeared on Science Friday
Dogs can smell silent, deadly cancers before a blood test can
Can doctors learn to detect the volatile compounds that dogs pick up?
We all go down our internet rabbit holes. For some of us, it’s news bloopers or cat fails. But for Jody Piltz-Seymour, an adjunct professor of ophthalmology at University of Pennsylvania and attending surgeon at Wills Eye Hospital just outside Philadelphia, it was seeking out the latest cancer detection research papers. She stole away any free time she could: when she got home from the office, on weekends, even at ophthalmology conferences. “My attention span would wane a little bit,” she laughs.
It wasn’t long before she came across a few curious papers in 2011. The research showed that dogs — with their superior noses — could be trained to detect the smell of cancer cells. “It made perfect sense to me,” she says. Dogs have been used for bomb-sniffing and search and rescue for years, thanks to their keen sense of smell and ability to be trained. “What didn't make perfect sense was that we weren't using that in any way in medicine,” Piltz-Seymour says.
Piltz-Seymour doesn’t have cancer and didn’t suspect she was sick either. But she was no stranger to understanding how the disease could wreak havoc on a person’s life.
“I grew up in a family where there was just cancer.”
Her grandmother, mother, aunt, and uncle all had breast cancer. The screening techniques caught the cancer in time for all of them except her uncle, who did not get screened. Ovarian cancer had also taken the lives of her father’s sister and her mother-in-law. Then, she lost her father to pancreatic cancer.
Doctors describe both ovarian and pancreatic cancer as “hidden.” They do not produce detectable symptoms until later stages of the disease, and slip past blood tests unnoticed. By the time it’s caught at those late stages, therapy isn’t effective. The odds of survival are slim.
Given her family’s history of cancer, early detection loomed large in Piltz-Seymour’s mind.
“Despite the passage of more than 20 years since their deaths, there were no clinically relevant advances made in the early detection of these cancers,” Piltz-Seymour says. She became restless and started making cold calls to relevant researchers to collaborate.
“That was very challenging,” Piltz-Seymour says. “Most people wouldn't take my calls. Most wouldn't return my emails. I mean, I'm an ophthalmologist calling them about using dogs. I think they thought I was crazy.”
The ultimate goal was to develop an instrument that mimicked the abilities of a dog’s nose — a tool to detect the undetectable.
And that’s exactly what a group of scientists in Philadelphia is trying to do — a group that Piltz-Seymour had a hand in assembling. Creating such a device — one that could save the thousands of patients who die from ovarian cancer every year — requires a specialized team: an oncologist, a chemist, an experimental nanophysicist, a veterinarian, and a band of highly-trained dogs.
Ovarian cancer ranks fifth in cancer deaths in women. The cancer first spreads in the ovaries, and by stage three and four, it runs rampant throughout the body. If and when the cancer is caught, the patient can have surgery to remove the cancerous cells. Then comes the chemotherapy.
“Many times, recurrences happen within the first couple of years, so then they're back in treatment, back in surgery, back in treatment. And subsequently, they become weaker and weaker,” says Lynn Franklin, volunteer president of the Kaleidoscope of Hope Ovarian Cancer Foundation.

Lynn Franklin (in green), volunteer president of the Kaleidoscope of Hope Foundation.
Daniel Peterschmidt
Franklin is an ovarian cancer survivor, but she didn’t know anything about the disease before she was diagnosed. That’s due in part to ovarian cancer’s relatively low number of survivors. “We do not have a large cadre of survivors that are out there fighting for the cause, like you have with breast cancer. The survival rate is so much greater in breast cancer.”
About 21,750 women will be diagnosed with ovarian cancer this year, according to the American Cancer Society. But about 13,940 — 64% — will die from the disease.
“This is a mean, mean disease,” says Janos Tanyi, an assistant professor of obstetrics and gynecology at the Hospital of the University of Pennsylvania. As a surgeon who performs 50 to 100 ovarian cancer-related surgeries each year, Tanyi knows the bleakness of the disease up close. He listens to Phil Collins to cut through the tension and high stakes of treating such a dismal disease.
“My life is ovarian cancer,” he admits. He squeezed in this interview between surgeries that day.
If a patient is diagnosed early, the cancer has a much better chance of being eradicated, since the disease at stage one and two are limited to the ovaries (94% of patients who are diagnosed early have a five year survival rate). But only about 15% of ovarian cancer cases are caught early.
Most common cancers have established early detection methods. For lung cancer, it’s a chest X-ray. For breast cancer, it’s a mammogram. But for ovarian cancer, there is none. The issue lies in its silent nature, proliferating with the faintest of symptoms.
These symptoms are nefarious in their normalcy. “It's a little bit of bloating. It's a little bit of indigestion, a little bit of discomfort. It's just really nonspecific,” says Cynthia Otto, director of the University of Pennsylvania Working Dog Center. And even if you are hyper-vigilant about your health and you go in for an exam, Otto says, doctors often don’t find anything wrong.
“It just doesn’t give a chance for the patient to be caught in an early stage,” Tanyi says. For years, the prospect of finding an early detection method for ovarian cancer seemed as grim as the disease itself. Then, starting in the late ‘80s, scientific papers started popping up, suggesting that dogs could smell cancer in their owners. For many scientists, like the late George Preti at the Monell Chemical Senses Center, the implications were clear and exciting. “If dogs can be trained to do it, we can do this with instrumentation.”
The whole reason Preti thought this research was possible was because of volatile organic compounds (VOCs). “Volatile compounds are things we encounter every day,” said Preti. “When you’re brewing coffee or cooking food, what you are smelling is a mixture of volatile chemical compounds emanating from the brewing coffee or the cooked food that gives it its nice aroma.”
And cancer cells, it turns out, have their own VOCs, their own unique smell, based on the types of chemicals found in those cells. Preti’s goal became clear: find the VOCs that are specific to ovarian cancer and make a “smelling” machine that can detect those chemicals from a sample of blood plasma, the clear part of the blood.

The blood plasma that the team uses.
Daniel Peterschmidt
The process starts with Tanyi. He provides not only the fundamental knowledge about ovarian cancer to the other researchers, but the plasma samples from the tumors that he collects during surgery. A patient will come into his office, suspecting that they might have a tumor, and Tanyi takes a blood sample.
“When I'm taking the blood, we don't even know that the patient has cancer,” Tanyi says. “We just have a suspicion.”
Later, the patient will have surgery and Tanyi can positively identify if the patient has a tumor and if it’s benign or malignant. If the patient consents to be part of the study, Tanyi distills the blood into blood plasma and sends those samples to the other researchers. So far, they’ve collected over 50 samples from ovarian cancer-positive patients.
But in the future, the researchers want to confirm the cancer without having to go under the knife. The goal is to “find an effective, dirt-cheap, screening methodology,” Tanyi says. “So, with a drop of blood, we will be able to identify if it's cancer-present or cancer-absent. That's all.”
Fortunately for the researchers, a smell detection device already exists to help them get started — it just happens to be furry, four-legged, and very adorable.
We’re gathered in a small testing room that feels cramped with more than five people. Among scientific charts and schedules, dozens of photos of dogs and their owners cover the cinder block walls. There’s a bumper sticker taped to the door that reads, “There is no such thing as a difficult dog, only an inexperienced owner.”
As entertaining as it is to stare at the memorabilia, the center of attention is a German shepherd named Ivey. She’s alert and focused, waiting for a command from her trainer. We’re all watching from behind a partition that splits the room in half so Ivey can’t see (or be influenced) by any humans. On the other side, lies a large metallic disk with eight prongs sticking out like spokes. At the end of each prong is a cup-like container covered with metal grates that hold individual samples.
This is the scent wheel. Ivey will walk around the wheel, smell each container, and see if she can smell which samples contain cancer and which don’t.
The researchers monitor a feed from a camera and as Ivey’s trainer gives her the command (“OK!”) to begin the test. She methodically puts her nose down to each sample cage, and pauses. If the sample doesn’t have cancer in it, she’ll stop very briefly and move on. If she smells cancer, she’ll pause longer until she hears a “click” from the trainer, confirming that she’s smelled correctly — if they’re in a training situation, explains Otto. In a true blind test, Otto and her team won’t know if the samples are positive or not.
Daniel Peterschmidt
“We have to just trust that if they say this is it, it's like OK, that one comes out as a positive,” says Otto.
Ivey completes her inspection of the wheel perfectly. She comes back onto our side of the partition, tail wagging excitedly as her trainer rewards her with a treat.
The Working Dog Center mainly trains dogs for search and rescue and bomb detection. Otto carried over her experience working with search and rescue dogs on the Pennsylvania Task Force One FEMA team, which she joined in 1993, and in New York City after the 9/11 attacks. But when she first started the center in 2012, one of her wish list items was to train dogs to smell cancer.
“So much of what our dogs do in search and rescue and law enforcement, it's all about saving lives,” says Otto. “It was just natural that we could put the dog's skills into [detecting cancer], and we also had evidence from several other publications that ovarian cancer did seem to have a unique odor.”
These super sniffers are designed to take in all the information in their environment, she says. The capacity for odor detection in dogs is reportedly 10,000 to 100,000 times better than in humans. (Not to mention that the olfactory center in the dog’s brain is about 40 times larger than in a human’s brain.)

Osa, a German Shepherd cancer sniffing dog.
Daniel Peterschmidt
“The dog's nose is so fantastic,” Otto exclaims. “I like to use the analogy that they smell in color. So as we see the world in color, and we see all sorts of different shapes, sizes, colors, and textures, that's how their nose is working.”
Their noses are so good that they only need 50 microliters of blood plasma — basically, just a tiny drop. “And it's really fun, because if you ask Preti how long it takes him to get a result from one of his samples, it's hours, if not longer,” Otto says. “You ask us how long it takes to get a result from one of our samples, you're going to see it.”
She snaps her fingers.
“Dog says yes. Dog says no. Done.”
In a couple sniffs, Otto’s dogs have the potential to save a human life. But she thinks dogs will only be seen in the research lab — not in your hospital room.
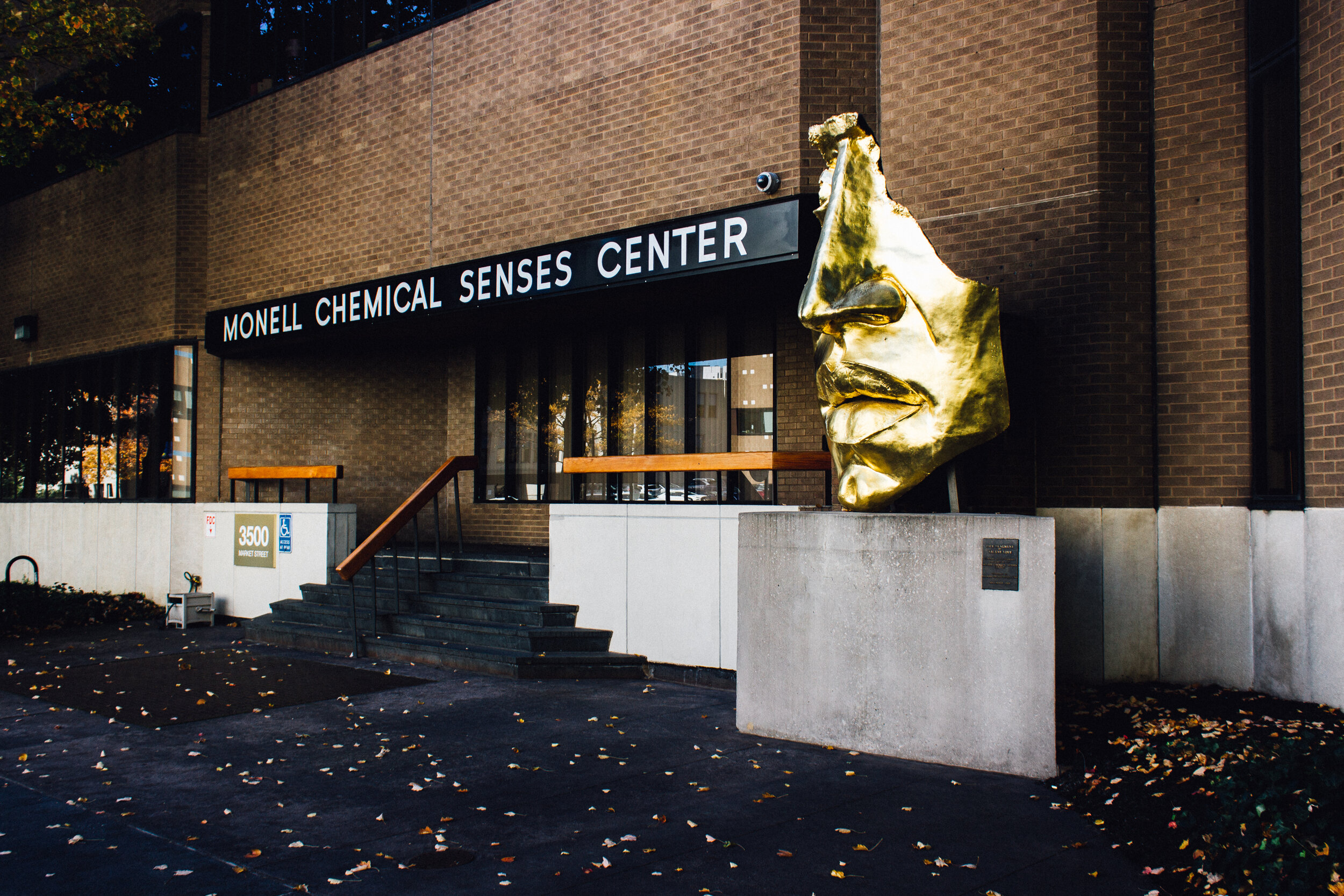
The Monell Chemical Senses Center, the home of George Preti's lab.
Daniel Peterschmidt
“For me, the relationship between humans and dogs is so important,” she says. That special relationship — between person and furry friend — is one of the reasons why Otto can’t imagine dogs will actually be used in the doctor’s office. If, for instance, a dog confirmed she had cancer, that connection would be spoiled.
“It would poison my bond with dogs,” she says. “I’d be like, no don’t come by me.”
That, among many other reasons, is why trained cancer-smelling dogs aren’t a routine part of every ovarian cancer patient’s diagnostic process. The dogs participate for treats and playtime, not for human health, Otto adds. There’s also only so much they can smell and process in a given time.
“They're using their brains so hard that after going through detecting 10 samples, they're like, ‘whoa, that was a lot of work.’ And they take a break,” she says. “I don't actually anticipate seeing dogs in laboratories or in medical centers because I think that they are a research tool to get us to that next step.”
The dogs are helping George Preti build a library of cancer VOCs — the smell profile of ovarian cancer. But how exactly do you figure out what chemicals are in a smell? The answer to that question lies within a building, two miles away from the Working Dog Center, that has a giant, golden human nose outside.
“It's deeply personal. I'm deeply pissed off.”
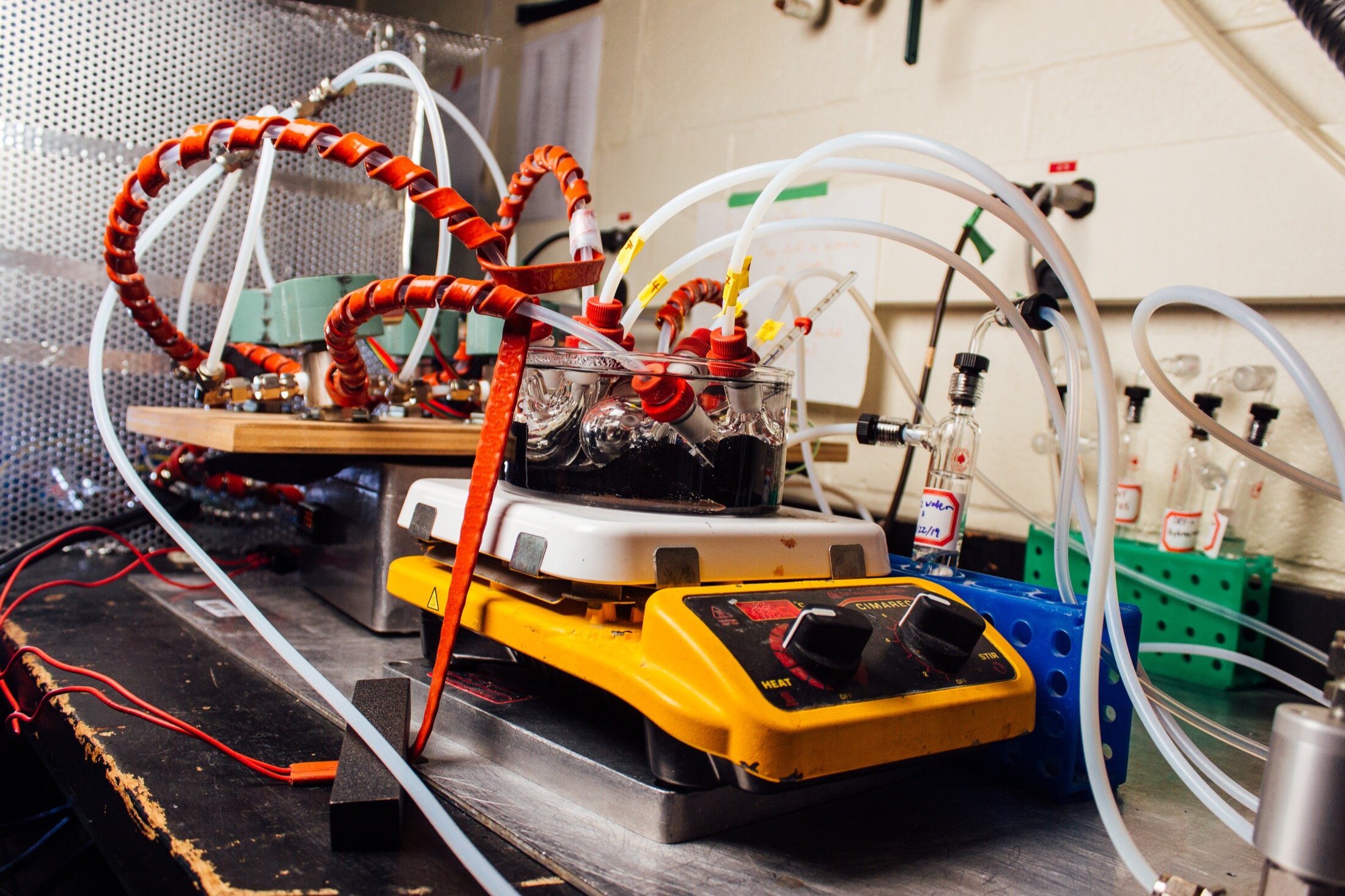
George Preti's lab at Monell Chemical Senses Center, a scientific institute that conducts smell and taste research, is the definition of “lived-in.” Every available surface and wall is covered by instrumentation, tubing, yellowing comic strips, and Star Wars figurines. Preti sat with his arms folded across his chest, wearing his glasses around his neck and a crease on his brow.
Daniel Peterschmidt
Preti didn’t know anything was amiss until he saw blood in his urine. His surgeon told him that he had been developing bladder cancer for two to three years. “I probably started growing the damn thing around the time I got my first grant to study ovarian cancer,” he recounted.
Bladder cancer, like ovarian cancer, often produces no noticeable symptoms until later stages. The irony of contracting a silent cancer while studying a silent cancer was not lost on him.
He had three surgeries, chemotherapy, and radiation oncology. At the time we met with him in October 2019, he was in remission, but the effects of radiation had a lasting impact. “I'd been so healthy,” he said. “I was in good physical condition. I used to weigh 180 pounds, and I weigh 140 after all the treatments I've gotten.”
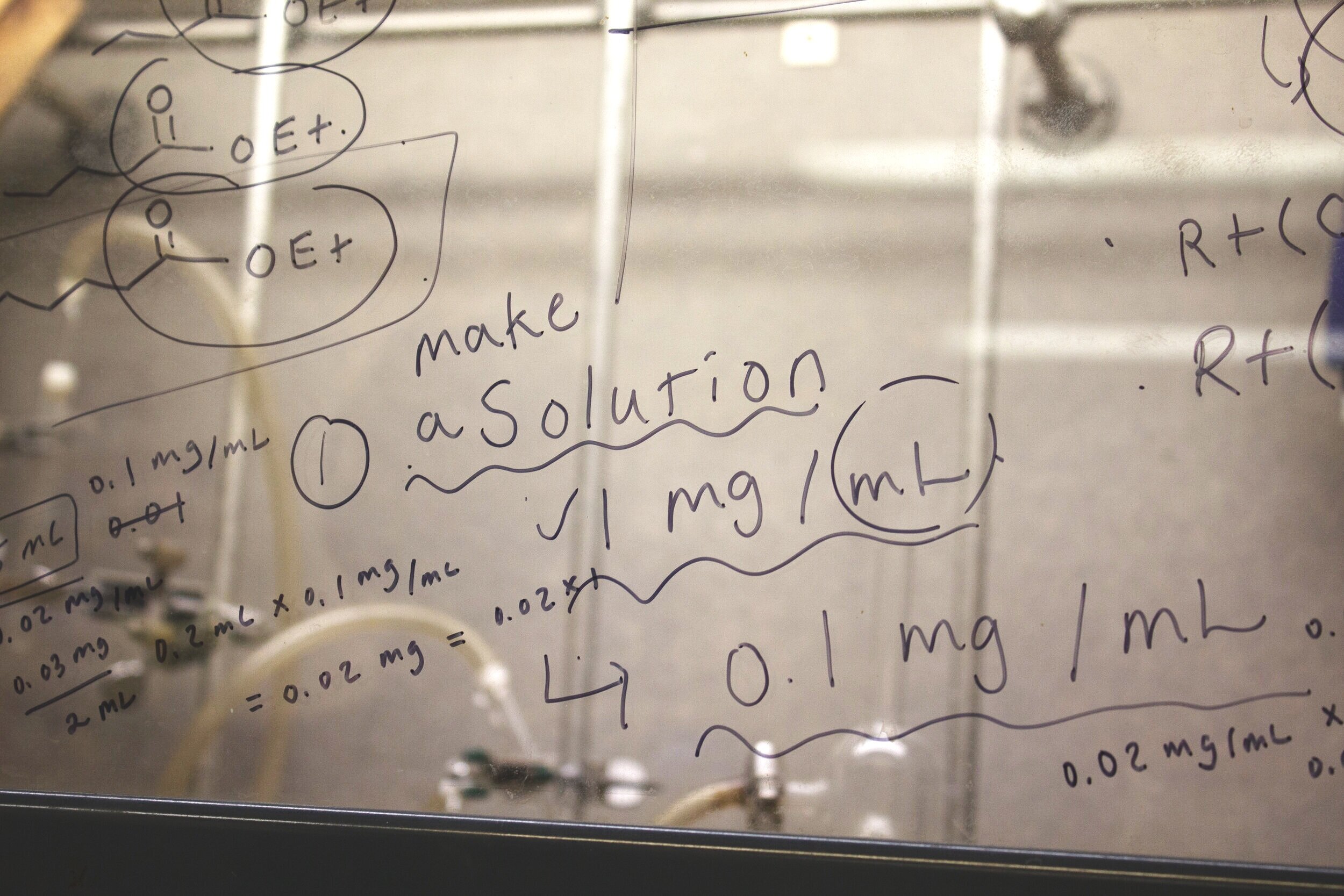
At the lab bench, Preti and his assistant showed us the instruments that he used to analyze the plasma samples processed in Tanyi’s office. Contained in the aroma wafting from the plasma is the project’s gold: the volatile organic compounds from ovarian cancer that Preti was trying to pick up.
Unlike something like armpit odor or citrus from an orange peel, it’s a lot harder to smell the VOCs emitted by ovarian cancer cells. And trust him — Preti tried.
“You may not be able to tell the difference between a cancer sample and a normal sample. At least I can't. And neither could my postdocs and I.”
In order to identify these VOCs, he used gas chromatography mass spectrometry (GC/MS) — a process that separates complex mixtures into individual chemical compounds. Then, Preti and his team must identify which of the compounds are specific to ovarian cancer. But sticking a sample in a machine won't magically give Preti all the answers. They have to reference literature, eliminate compounds that are associated with metabolism, and take into account the patient’s age, health, and medical history. Out of 110 VOCs, they’ve isolated 28 so far and plan on finding more.
Still, there is room for error, Preti said. His chromatography and spectroscopy machines are, undoubtedly, helpful and necessary tools in creating a comprehensive chemical profile for ovarian cancer. But they spit out thousands of different chemicals that lie within the ovarian cancer blood sample — and almost all of those chemicals have nothing to do with ovarian cancer.
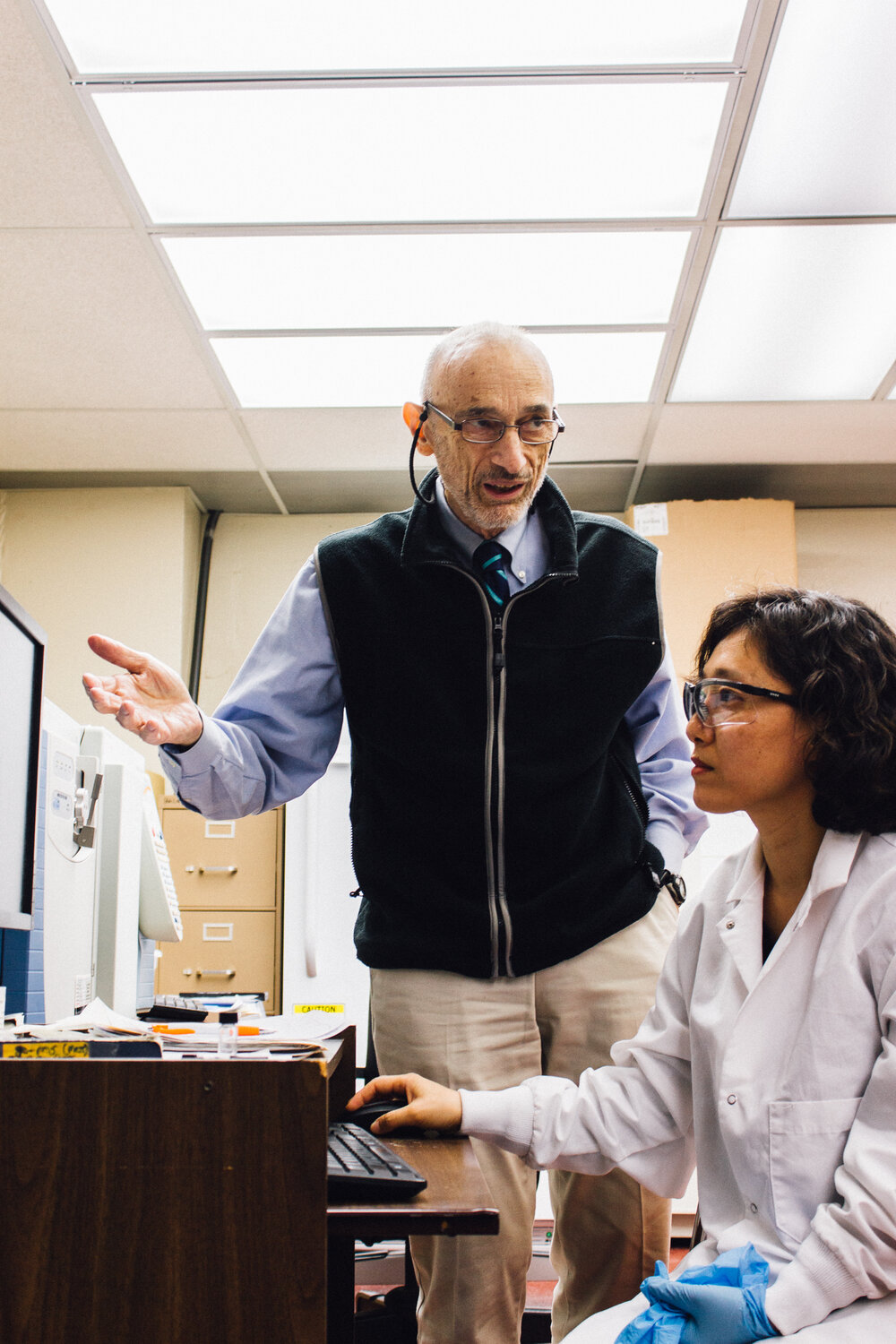
George Preti with his research assistant, Young Lee.
Daniel Peterschmidt
“When we're looking at the chemistry, it really is challenging,” says Otto. “The dogs have no problem figuring out the subtle differences.”
After Preti completes this analysis and labels which samples he thinks are cancer-positive, he will make mixtures of different amounts of just those VOCs and send it to Otto’s lab. Otto’s dogs will narrow the correct VOCs even further. The dogs smell those and give a “yes” or a “no” or a “maybe.” Then she’ll pass the suspected dog-approved cancer VOCs over to Charlie Johnson’s lab at UPenn so he can tell his machine exactly what to look for.
“If we could come up with an instrument that was as good as a dog, or even approached a dog, I think in the long run that would be a better solution,” Johnson says. And that’s exactly what he’s done.
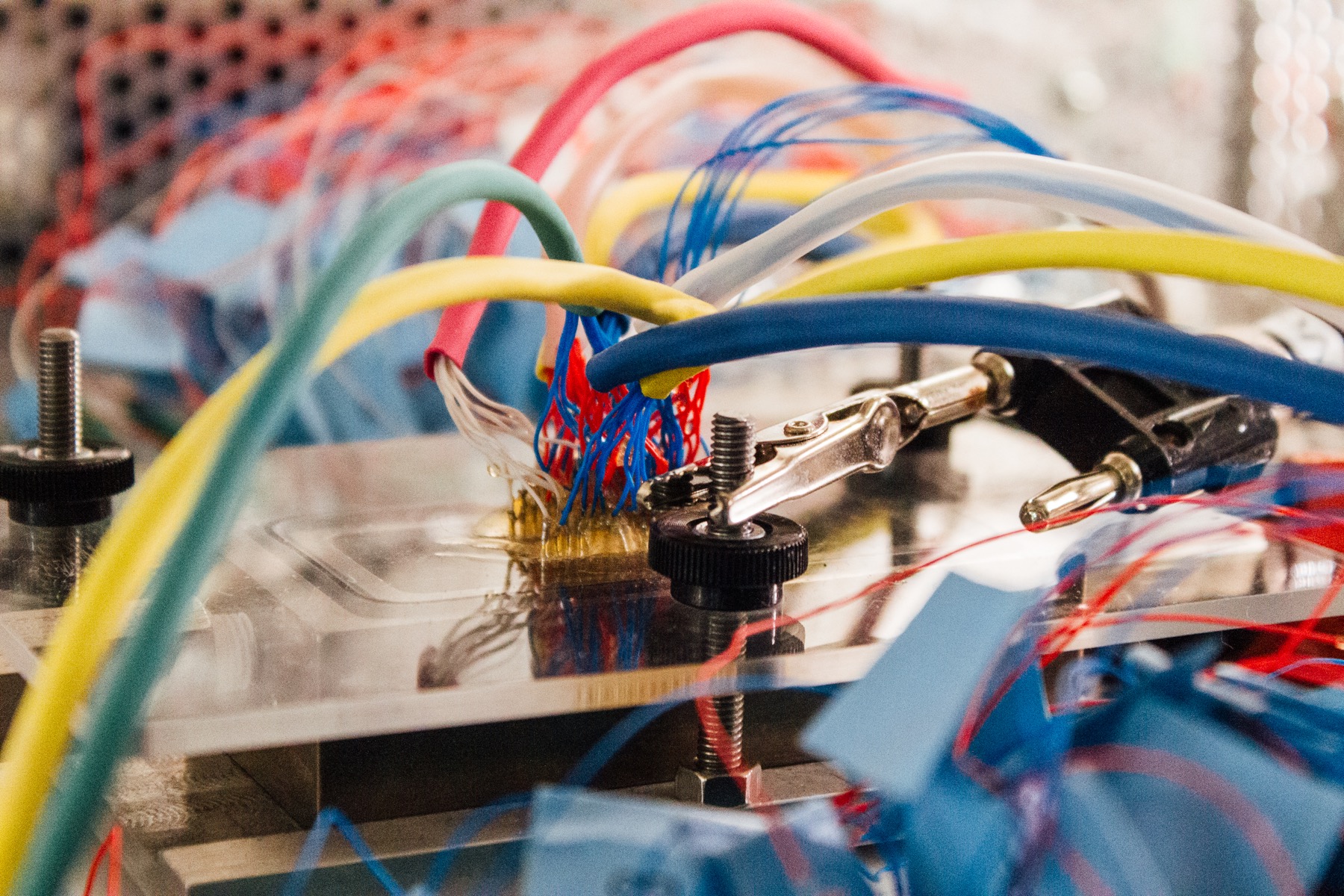
In the basement of UPenn’s physics and astronomy building, a contraption bubbles and hums on a lab bench. There are translucent tubes, curling multi-colored wires, and an inky-black liquid. Dozens and dozens of the wires flow onto a tiny chip, surrounded by an imposing metal cage. It gurgles and wheezes and almost seems alive.
The apparatus essentially replicates an animal’s nose. Johnson’s machine is the culmination of the research that Otto, Tanyi, and Preti have been working on. It’s a prototype, but it works — mostly.
“Our system is much simpler than what's happening in the animals, but it seems to be working very effectively.”
While it’s not furry or cuddly like Otto’s cancer sniffers, you begin to appreciate the machine’s character the closer you look — down to an atomic level. Johnson’s detection machine is a work of molecular manipulation. He and his lab harnessed the powers of a “wonder” material: carbon nanotubes. They look like “black lint like you might pick out of your pocket after a day,” says Johnson, but the material is much stronger than loose fabric.
Carbon nanotubes, discovered in the ‘90s, were originally hailed as a super material. Only one atom thick, the hexagonal, chicken-wire structure the carbon atoms form is incredibly strong. Material physicists were dazzled by its potential applications, imagining super-strong, super-light vehicles, bridges — even elevators to space.
Daniel Peterschmidt
Today, those grand visions haven’t exactly panned out. Scientists haven’t been able to manufacture them on the scale that you would need for, say, a space elevator. But they have been able to make them in small amounts — and as Johnson found out, the applications for carbon nanotubes go beyond building materials. “It turns out that DNA is very happy to interact with carbon nanotubes and it interacts in a very gentle way,” he says. “So you can easily form a layer of DNA that's in contact with a carbon nanotube while the carbon nanotube is undamaged.”
You can think of the layers like the delicious combination of peanut butter and chocolate, he says.
“Sometimes I say that DNA and carbon nanotubes, they're like the Reese's peanut butter cup of nanotechnology,” says Johnson. “Each one is terrific on its own, and together it's something that's just great.”
This “Reese’s peanut butter cup” mixture gives carbon nanotubes a special set of reactive properties. Johnson and his team waft vapors from the blood plasma samples over the DNA-paired carbon nanotubes, which lie on top of a silicon wafer connected to a computer. Depending on what VOCs are in the vapor, it will trigger a certain pattern of electrical charges that is passed through the carbon nanotubes and is detected by the silicon wafer, which sends those charges to the computer. Depending on the type or amount of VOCs present in the vapor sample, the pattern of electrical charges will be different — telling Johnson’s team if a sample is ovarian cancer-positive or not.
At this stage, the prototype is still not up to snuff. “The dogs are still the best,” Johnson admits, but adds, “We have a system that can detect correctly somewhere between 90% and 95% of the time.”
But despite the high success rate, there’s still more to be done. Right now, they have a good idea of what compounds are in the vapor, but the team wants to get more specific. One of their big goals is to be able to distinguish between early- and late-stage cancer. “It would be incredible to identify these people at an early stage and really having an impact on saving lives,” says Otto. “That's what we really want, and the dogs have been able to detect that. We need more samples to make sure that that's consistent.”
Daniel Peterschmidt
“If you could tell if someone might have the beginning of a cancer from an odor test such as this, that would certainly set them up to go back to the doctor for further testing and further analysis,” Johnson says. That blood test could then be rolled in as part of your annual checkup, making some hidden cancers a thing of the past.
But the road to that destination isn’t smoothly paved. The biggest obstacle the team faces is not narrowing down the VOCs. It’s money. “Right now, it really is a matter of research funding. And we are working very hard to get over that,” Johnson says.
During her childhood, Piltz-Seymour watched her grandmother struggle with breast cancer. “She had a radical mastectomy. So, I grew up with a grandmother that only had one breast. And I mean, it was just kind of normal in our family.”
Today, cancer continues to be a part of her life, but in a more productive and constructive way.
After connecting Otto to the rest of the team, she continued to play a role in moving the research along. She sets up blood drives to obtain control samples (“I have collected 268 samples to date!” Piltz-Seymour says). And she helps write papers about the research that’ll be submitted to scientific journals. It’s even become a family effort.
“My husband and my daughters have always been very, very supportive of the project. Specifically when I was cold calling people, they would be like, ‘Keep going Mom!’” she says. “Actually, my older daughter is helping me format the manuscript, a submission into a journal. In fact, as we speak, I believe.”
Needless to say, Piltz-Seymour has been fully adopted into Tanyi, Otto, Preti, and Johnson’s team.
Together, they’ve come a long way since 2012. They have a good idea of what VOCs are in an ovarian cancer cell and they’ve built a smelling machine that can detect those chemicals. Now, they just need more samples (and more funding) so they can improve the machine and distinguish between early and late stage cancer. Currently in hospitals, “we don’t have the screening tool. And this is why the research is extremely important,” says Tanyi. “This is a horrible disease and the only way to save lives is to catch it early.”
“Many of us involved in this project know people who were affected [by ovarian cancer] in this way,” Johnson says. “The ability to do science that might actually improve the world in some really tangible way is a rare opportunity. So it's nice to get out of bed in the morning and think, that's what I'm going to try to do today.”
On March 3, 2020, George Preti died after a long battle with bladder cancer. His research into the detection of hidden cancers and other diseases continues. The newly established George Preti Research Support Core for Analytical Chemistry will share his foundational scientific resources and wisdom to the whole of the Monell Center and its international collaborators. Memorial donations can be made to the George Preti Research Support Core for Analytical Chemistry.
Written, photographed, and designed by Daniel Peterschmidt
Video produced by Luke Groskin
Reported by Daniel Peterschmidt and Luke Groskin
Edited by Lauren J. Young, with additional story edits by Nadja Oertelt
Fact-checking by Kaitlyn Schwalje
Music by Audio Network
Additional Stills by Shutterstock
Dog Nasal Cavity MRI Courtesy of Brent Craven
Special thanks to Christian Skotte, Brandon Echter, Danielle Dana, Christie Taylor, and the rest of the Science Friday staff. Thanks also to Young Lee, Karen Kreeger, Martin J. Hackett, Erica K. Brockmeier, Amanda Mott, Andrew Malloy, Vicki Berkowitz, and Terence Collins.
