It's time to track city sewage for emerging diseases, not just COVID-19
The current pandemic accelerated the wastewater epidemiology techniques, but researchers hope to continue the practice to prevent the next one
Zeynep Çetecioğlu wants to create a cleaner, more sustainable society by finding better ways of dealing with the waste it creates.
Çetecioğlu's work focuses on the wastewater that flows through the city sewers. Wastewater and the semi-solid sludge that forms when it is cleaned are rich in organic molecules that can be used as fuel or feedstock for making bioplastics. Wastewater is also full of molecules and microbes that tell stories about how a society lives, and about the health of a city’s inhabitants. Monitoring wastewater can predict and prevent a variety of disease outbreaks. But despite a wealth of new scientific evidence, this potentially powerful epidemiological tool depends crucially on government support that often falls short.
In spring 2020, as the COVID-19 pandemic escalated, scientists around the world pivoted to working from home as best they could, often putting research projects on hold. Çetecioğlu and her colleagues at Stockholm’s KTH Royal Institute of Technology knew that the virus’s genetic material (RNA) could be detected in human waste, and had seen some exciting early results from a pioneering wastewater group in the Netherlands, who were the first to show they could detect RNA from SARS-CoV-2, the virus that causes COVID-19.
Çetecioğlu is co-lead on a project that’s tracking SARS-CoV-2 RNA in wastewater. The technology can give cities advance warning of an increase in COVID-19 cases before sufficient infected people can be tested. The second wave of infections in Stockholm was predicted by Çetecioğlu and her team, who saw a clear increase in RNA in wastewater sampled two to three weeks before positive tests started increasing. In a press release from early October, Çetecioğlu said, "The data from August and September show that...there’s more virus in the population."
The method for detecting viral material in wastewater uses simple molecular biology techniques. The RNA is extracted from the water, then detected by polymerase chain reaction, or PCR, the same test used to detect COVID-19 in human patients. Scientists use equipment that gives a real-time read-out of the RNA concentration in a sample being analyzed.
The tricky part is making sure you have enough virus to detect by PCR. Wastewater treatment plants process enormous volumes of liquid, so viral particles shed by a few people become very dilute. The method used to concentrate the viral material needs to be optimized depending on whether the virus is “enveloped” or not. (Like other coronaviruses, SARS-CoV-2's RNA genome is surrounded and protected by a membrane envelope.) Existing virus concentrating methods developed for non-enveloped viruses therefore had to be modified.
The group in Stockholm recently compared four different methods of concentrating viral RNA. The main differences between the methods are whether they use ultra-filtration — passing water samples through filters made from cellulose membranes that only allow tiny RNA particles through — or if they absorb the virus onto a solid material from which it can be collected by washing. They focused on using chemical reagents that are inexpensive and unlikely to run short in labs even if deliveries are delayed during the pandemic.
Their results showed that the ultra-fitration method consistently recovers the most virus, and that it can be applied to wastewater from different European cities. Çetecioğlu says that the scientific challenges involved in detecting and measuring SARS-CoV-2 RNA in wastewater are now largely settled, as the method has been validated in many places (follow COVIDPoops for updates). It has also been used to look for other viruses, including a mouse hepatitis strain and a plant virus used as a water quality indicator. In Gothenburg in 2017, PCR was used to track an outbreak of a winter vomiting virus, or Norovirus. That pathogen was detected in wastewater before the outbreak had been noticed by local healthcare providers, so hospitals and elder care homes had time to prepare.
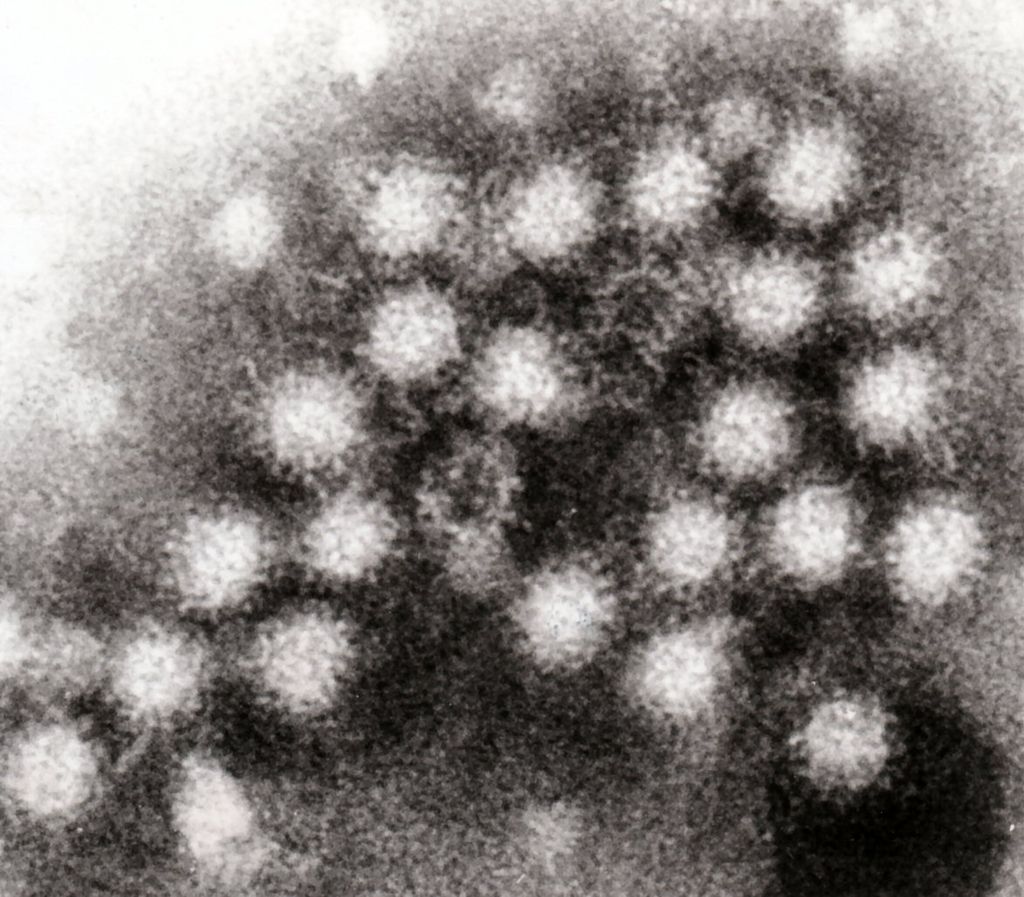
A 2017 effort helped predict a Norovirus outbreak based on wastewater
Wikimedia
The SARS-CoV-2 genetic sequence was first released in January 2020. The research group in the Netherlands who started the first COVID-19 wastewater project were collecting and testing samples before there was ever a positive case in that country. This was possible because there had been advance investment in a wastewater epidemiology lab that could leap into action as soon as the sequence was known.
The Swedish team is generating high-quality data, but have not been able to release results weekly as they had hoped, due to frequent delays in sample testing. “We receive the samples every Monday and Tuesday, but we can’t share the data every Wednesday,” says Çetecioğlu. “It is partly about lack of personnel, but also because of the simplest things, like now we have no gloves, or now we have no filters.” Deliveries of small items that ordinarily arrive after a few days are now taking months to arrive.
Other scientists in the project have discussed the need for support if the method is to be scaled up to serve as the city’s early warning system. With full-time staff, and priority access to equipment, a dedicated wastewater epidemiology lab could release weekly statistics on the viral content of local wastewater, focusing on outflows from healthcare centers to monitor vulnerable groups, and adding novel viruses into their analytical panel as soon as a new sequence and extraction method were available. Researchers from Yale University have confirmed that wastewater testing can give public health organizations at least a week’s notice of an increase in cases of a known virus, and stressed the value of this in places with delayed patient testing.
“We need to scientifically approach each new viral outbreak as a new wastewater problem, optimizing extraction and detection methods everywhere, as soon as a new pathogen is discovered somewhere in the world,” says Çetecioğlu. But the potential power of wastewater monitoring as an early warning system requires us to be ready to implement it before a local outbreak takes hold. “I started this work for the public. I am not doing this for my career. We are producing data and methods for the city to use in the future.”
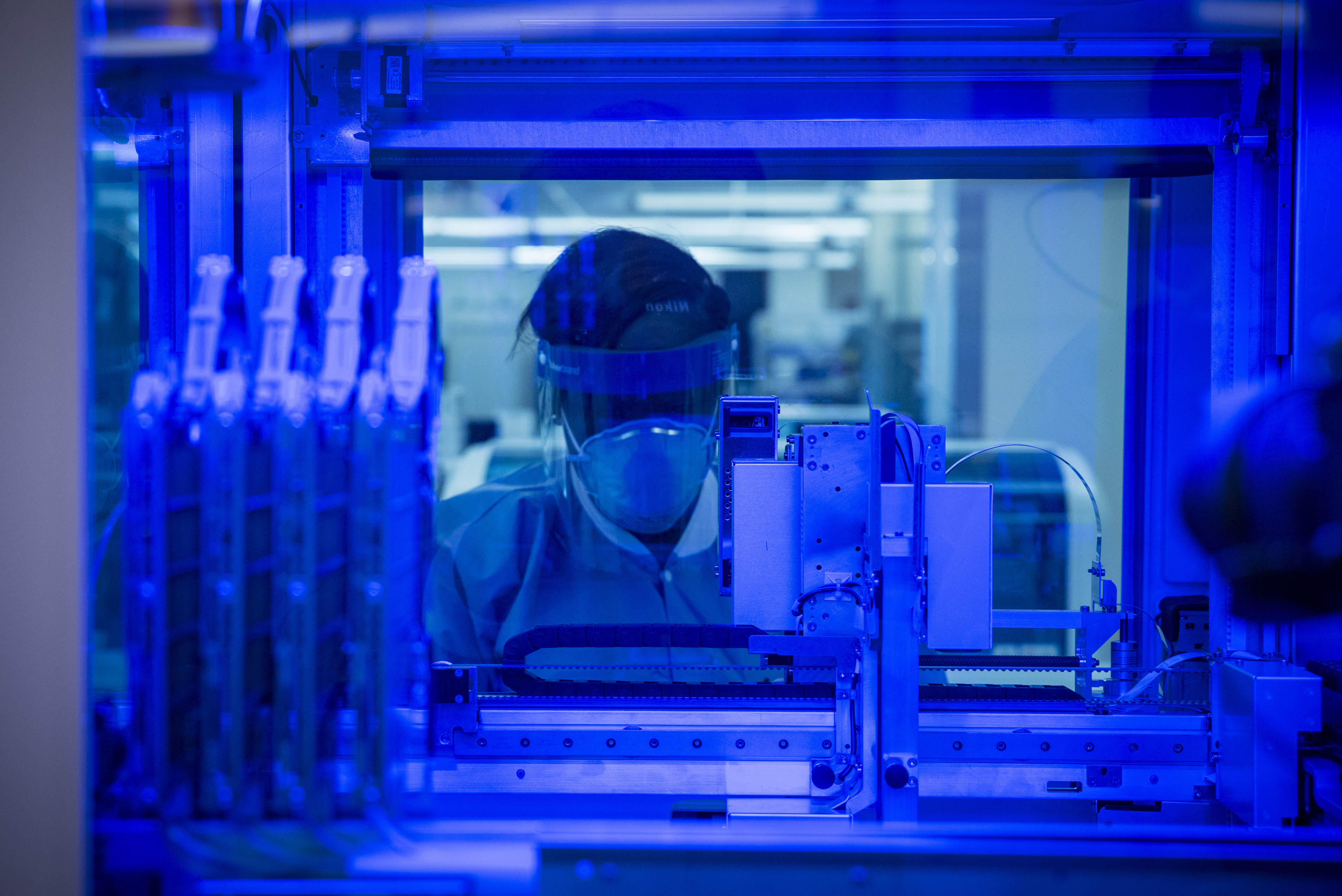
Biological testing supplies have limited the Swedish team's effort to report wastewater test result
U.S. Air Force photo by Richard Eldridge
Not everyone agrees about the value of wastewater epidemiology. Anders Tegnell, state epidemiologist, has been coordinating the Swedish response to COVID-19. He has become a pretty controversial character, taking Sweden down a different path than its European neighbors. In an interview with Swedish newspaper Dagens Nyheter, Tegnell said that wastewater testing was scientifically interesting, but offered no new information to help him manage the outbreak, as it only supported what he already knew from patient testing — that case numbers were rising.
Of course, with access to enough lab supplies, the Swedish team likely would have been able to show SARS-CoV-2 RNA in wastewater weeks before diagnoses started climbing. Samples collected in April couldn’t be analyzed until May, when case numbers already began rising. The same delays hit the lab in late summer, but SARS-CoV-2 RNA levels were high in wastewater collected a month before case numbers started rising in the autumn.
Çetecioğlu and her colleagues were recently awarded funding from the city of Stockholm and some private Swedish foundations. These funds should pay the salary of a dedicated scientist to work on the environmental virus profiling project, help build a viral biobank for the future, and allow sequencing studies to track mutations.
“Today the problem is Covid-19,” Çetecioğlu says. “Tomorrow there will be a different problem.” We will face pandemic diseases increasingly often in the future, as they are made more likely by our destruction of the natural world. Governments need to focus on pandemic preparedness, and an element of this should be the establishment of well-resourced wastewater epidemiology labs in those areas that see the most rapid spread of pathogens, like densely populated cities. We need to be ready.
Disclosure: the author of this article is employed by KTH, Royal Institute of Technology, where the interviewee Zeynep Çetecioğlu is an Associate Professor. They work in different departments and do not share any resources or project funding.



This is a fascinating article - I love the idea that we can use wastewater to monitor things like drugs or diseases. I’m a chemist, not an epidemiologist, so I have a question about the timescale of using wastewater to identify an emerging disease.
When studying the waste water, how can epidemiologists identify if a species present in the waste water is something that will potentially pose a problem in society as an infectious disease? For example, you mention that SARS CoV-2 RNA levels were high in wastewater weeks before diagnoses increased, but you can’t measure those levels without performing diagnoses and identifying the infectious proteins.
If a brand new infectious disease was to arise right now, how long would it take to characterize and identify the disease before wastewater could be used as a reliable source to track emerging diseases? How long is a disease classified as emerging?