Why designer mental health drugs are still elusive
The fruitless, decade-long search for DREADDs has a silver lining
Mental illnesses are incredibly challenging to treat. Our brains all react to medicine differently, and even when scientists think they’ve nailed down a key chemical, it often turns out to have a variety of effects. Although we researchers think that serotonin deficiencies contribute to depression in certain individuals, for example, increasing serotonin in the whole brain can have many unintended consequences.
For this reason, we need treatments that can target specific brain areas or even cell types. Such technology would allow us to specifically target brain regions and manipulate them, first for research in non-human models, and ultimately for clinical use. Designing a tool that is specific and safe enough to work in primates or humans is – not surprisingly – an enormous and complicated task.
In 2007, Brian Roth and his lab published a paper describing such a dream technology. It was a lock-and-key system that combined chemistry and genetics, often termed “chemogenetics.” They designed a receptor to put into the membrane of a cell to either increase or decrease that cell's activity. In addition, they found a perfect key–a chemical called clozapine N-oxide, or CNO–to open that receptor. Roth’s lab didn’t dive into the mechanisms of the lock and the CNO key; they simply observed that when you gave the drug to animals, it would cause a change in behavior.
They called the technique “Designer receptors exclusively activated by designer drugs,” or DREADDs for short. Since then, the use of DREADDs in neuroscience research has skyrocketed, with more than 800 studies reporting the use of the technology.
But it turns out DREADDs don't work they way we thought they did. Truthfully, no one had really nailed down a complete explanation of the system until a group of scientists from the National Institute on Drug Abuse (NIDA), led by Michael Michaelides, came along. Their research, published this year, shows that the key to the DREADDs receptor might not actually be CNO. It's a good reminder that tinkering with the brain is difficult – even introducing one chemical into the body can have unexpected consequences.

DREADDs study author Mike Michaelides
When CNO enters the body, it's processed into several different components, or metabolites. First, the Michaelides crew tested the ability of CNO and its metabolites to bind to the DREADDs receptor. Importantly, they didn't just do these binding tests in isolated cells. They also tested CNO and its metabolites in living mice, mirroring the way DREADDs is typically used in the laboratory.
It turns out that CNO doesn't even bind to the DREADDs receptor, making its ability to alter behavior quite mysterious. It’s not the drug itself – many labs have given animals CNO without any DREADDs and didn't see any effect. So CNO is having an effect on the brain and behavior, but not directly. Something else was working on the lock-and-key receptor.
It was actually clozapine, a known depressant, that could cross the blood-brain barrier and bind to DREADDs receptors in the brain. With all of this evidence, the Michaelides group concluded that clozapine was actually the culprit that snuck into the brain to activate DREADDs receptors. The behavioral impact of DREADDs was actually thanks to the clozapine, not the CNO.
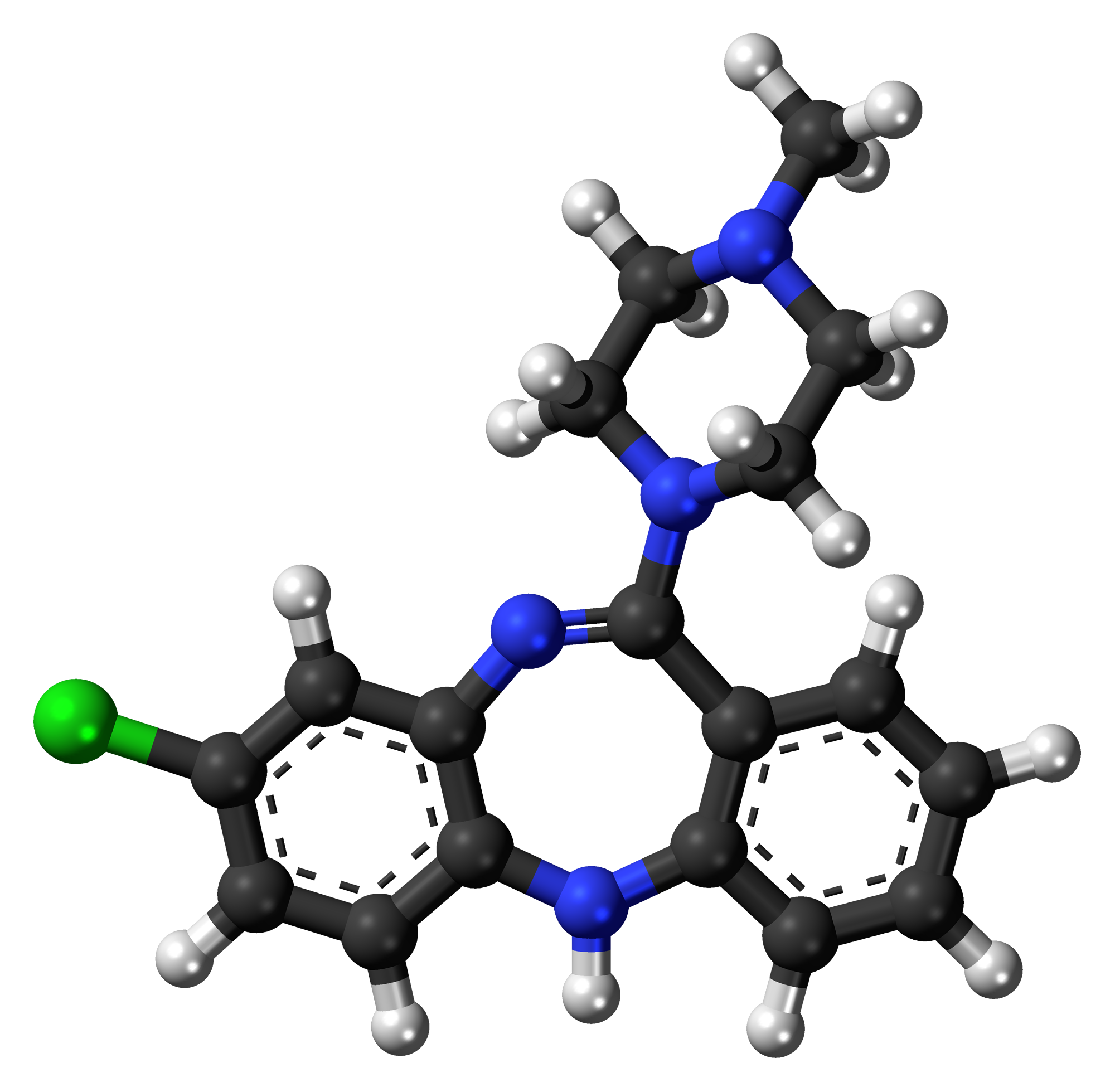
A clozapine molecule
This is potentially problematic because clozapine is a known sedative with effects on other receptors in the brain, meaning it could complicate the whole goal of finding a way to target cells in a very narrow, specific way. However, there is good news: clozapine can bind to DREADDs receptors at super low concentrations. This means we should be able to use clozapine to activate DREADDs without any off-target effects.
Since the main effects of DREADDs technology seems to be due to the metabolism of CNO to clozapine, and this metabolism can vary across individuals, the authors conclude that researchers should use low doses of clozapine as the pharmacological agent, rather than CNO. In this way, they would be controlling the known culprit in the DREADDs system, and reduce off-target effects of CNO.
Although this report shook up the neuroscience community, it actually has promising implications for DREADDs as a therapeutic. Clozapine is already approved by the Food & Drug Administration for use in humans and it has been used clinically for decades as an antipsychotic medication. DREADDs works, just not the way we thought. Researchers will need to do a lot of work in order to safely introduce DREADDs receptors into human brains, but it is theoretically possible with the use of safe viruses that can infect cells but don’t have any side effects.
Ultimately, this paper is a shift in thinking for neuroscientists, but a promising step forward for a technology that could help treat complicated mental disorders.
