
Ake via Rawpixel
What do we really know about the safety of probiotics?
Messing with our gut microbiome could hurt us
In a given year, nearly 4 million Americans use probiotics or prebiotics. Though sometimes used as synonyms, probiotics are live microorganisms, and prebiotics are essentially food for these “good” bacteria; proponents claim these supplements can balance your digestive system, boost immunity, and support metabolism. But do they actually make you healthier? It’s hard to say. In some cases, probiotics may be effective at treating or preventing disease, but some studies show probiotics may do more harm than good. New research by an international collaboration highlights this lack of data on the potential side-effects of probiotics.
Individual studies with small numbers of participants have found that probiotics can do everything from improving autism symptoms to reducing the risk of certain skin disorders. But many of these studies lack proper control groups, and so their results may be substantially influenced by the placebo effect.
In fact, meta-analyses—statistically combining data from multiple studies—of probiotics indicate that there is insufficient evidence to support the effectiveness of probiotics in treating or preventing most conditions. These analyses found that there was not enough evidence to support probiotics' impact on preterm labor, Crohn’s disease, urinary tract infections, and more.
To make matters worse, the kinds of probiotics you can get at the health food store are not regulated, meaning they might not be accurately labeled or standardized. For example, two different batches of a commercially available probiotic mixture called VSL#3 were shown to have markedly different levels of efficacy in the treatment of a mouse model of colitis. Even when products contain the bacteria listed on the labels, it is often unclear whether they remain viable after exposure to stomach acid.
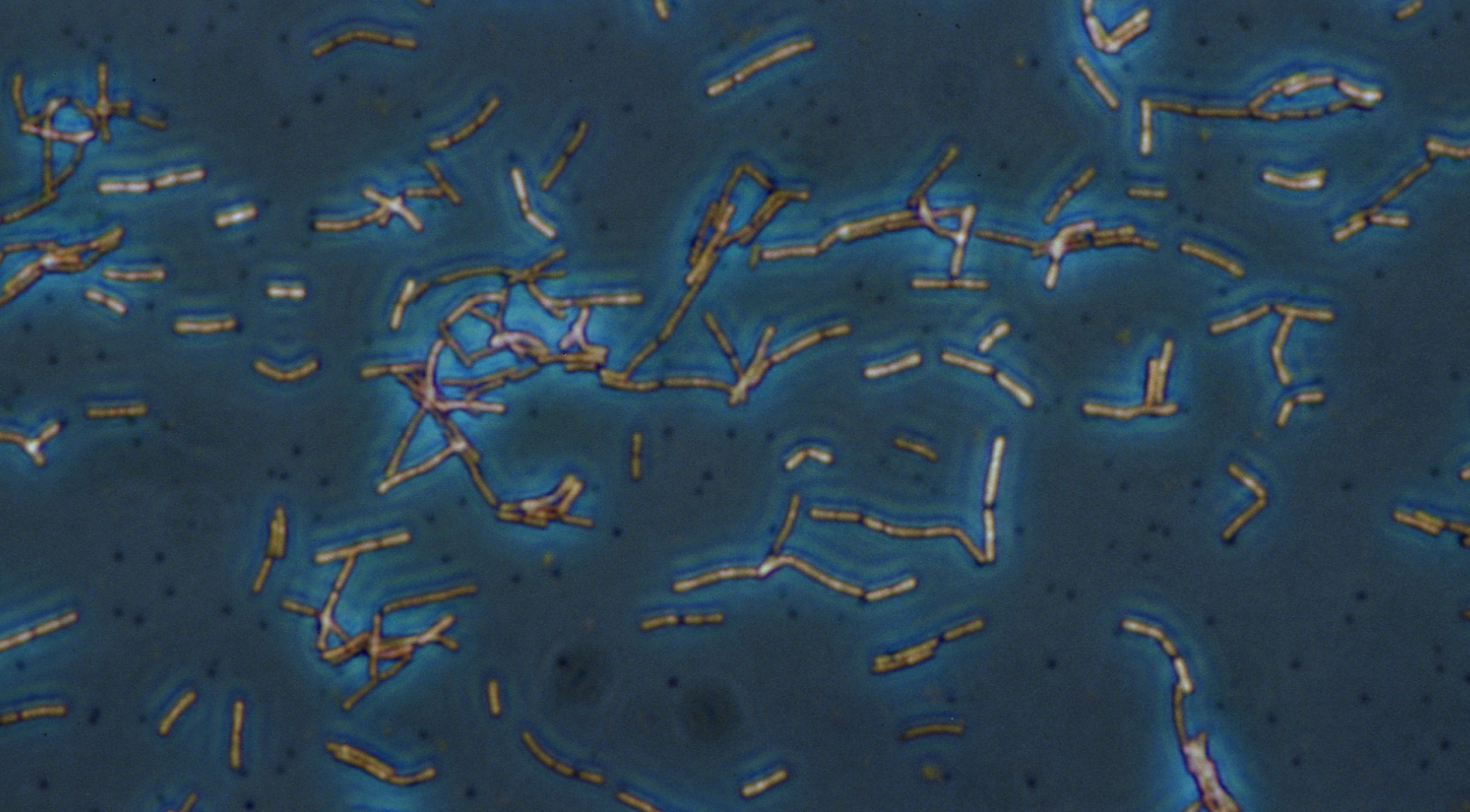
Yum, Lactobacillus acidophilus.
But so what if probiotics aren’t always all they're cracked up to be? Proponents argue that at least, unlike pharmaceuticals, they don’t have harmful side effects. In fact, we know very little about probiotic side effects. Because probiotics are generally considered safe, there's been relatively little effort to understand their potential side effects. In a recent evaluation of 384 randomized controlled clinical trials that aimed to alter the microbiome (using probiotics, prebiotics, or a combination of the two), many contained little to no information on side-effects. A staggering seventy percent of these trials did not report the number of patients who left the trial due to adverse events, like negative side effects. That's wildly different than, say, new cancer drugs, which must have highly detailed reports of safety in large numbers of patients before they can be approved by the FDA.
Preliminary research shows that in certain cases, probiotics can be detrimental. Many clinicians recommend taking probiotics after a course of antibiotics to “rebalance” the gut microbiome. But a 2018 study in Cell actually found the opposite effect: In both humans and mice, taking probiotics delayed the recovery of the gut microbiome to its pre-antibiotic state. While this study had fairly small numbers of human participants and will need to be replicated, it is certainly a challenge to the prevailing opinions on probiotics. Even more shockingly, a 2008 study of probiotics in 296 patients with severe acute pancreatitis found that probiotic treatment significantly increased the risk of death compared to the placebo group.

This is not to say that healthy people should be worried their probiotics might kill them. It simply shows that we cannot assume that probiotics are safe in all circumstances and in all patient populations.
On the whole, scientists agree that the gut microbiome plays an essential role in human health, potentially influencing our risk for digestive, autoimmune, and even neurological disorders. But the gut contains hundreds of species of microbes, and the role that each species plays in health and disease is far from clear.

Just say no to kombucha?
Photo by Klara Avsenik
Most studies, for instance, find that the gut microbiome of patients with Parkinson’s disease is significantly different from healthy controls. But there is still no consensus on exactly which types of bacteria are altered. One study will find a significant decrease in the genus Prevotella and an increase in the genus Bifidobacterium in Parkinson's patients, another will find no difference between Parkinson's patients and healthy controls in either genus. Some studies find that Parkinson's patients have significantly less short chain fatty acids (SCFAs), a metabolic product of gut bacteria. This has led to hypothesis that a lack of these fatty acids may contribute to some of the symptoms of Parkinson's. But another study (albeit in mice) seems to suggest that SCFAs actually contribute to the disease's progression.
If we don’t know which species—or which metabolic byproducts—contribute to disease, how can we know what sorts of bacteria should go into a probiotic treatment? It seems that we could be as likely to exacerbate the disease as treat it.
Probiotics aren’t inherently dangerous, but they aren’t inherently safe either. It will likely be decades before we have a complete understanding of the human microbiome. In the meantime, we should perhaps use probiotics with more caution.



Many assume anything marked with “probiotics” is good for you, but as Hannah Thomasy wrote, it’s not always the case. The study mentioned here on taking probiotics after antibiotic treatment is particularly fascinating to me. Because our microbiomes are so different - maybe one day, we’d be able to personalize the probiotics we take so that they better match the make up of our microbiome. I’d like to see how taking “personalized probiotics” affect our recovery of the gut microbiome after taking antibiotics.